Methamphetamine
Methamphetamine (also called meth, crystal, chalk, and ice, among other terms) is an extremely addictive stimulant drug that is chemically similar to amphetamine. It takes the form of a white, odorless, bitter-tasting crystalline powder.
Methamphetamine is taken orally, smoked, snorted, or dissolved in water or alcohol and injected. Smoking or injecting the drug delivers it very quickly to the brain, where it produces an immediate, intense euphoria. Because the pleasure also fades quickly, users often take repeated doses, in a “binge and crash” pattern.
Methamphetamine increases the amount of the neurotransmitter dopamine, leading to high levels of that chemical in the brain. Dopamine is involved in reward, motivation, the experience of pleasure, and motor function. Methamphetamine’s ability to release dopamine rapidly in reward regions of the brain produces the euphoric “rush” or “flash” that many users experience. Repeated methamphetamine use can easily lead to addiction—a chronic, relapsing disease characterized by compulsive drug seeking and use.
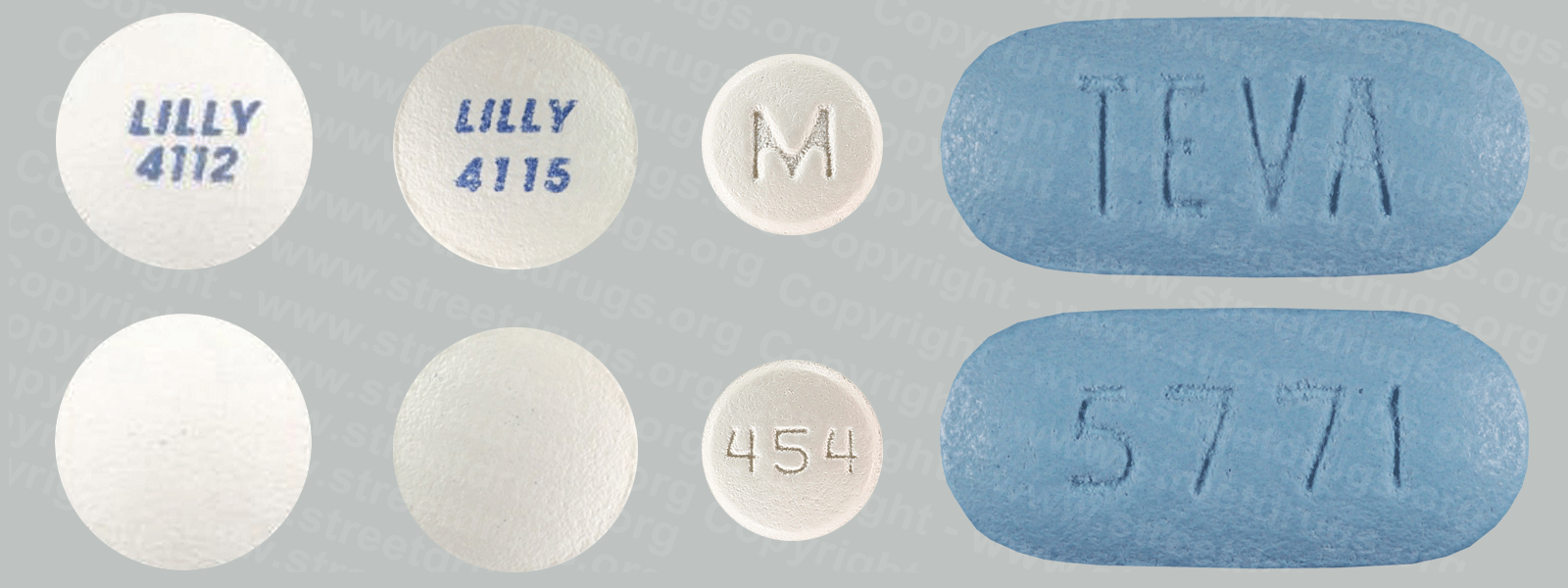
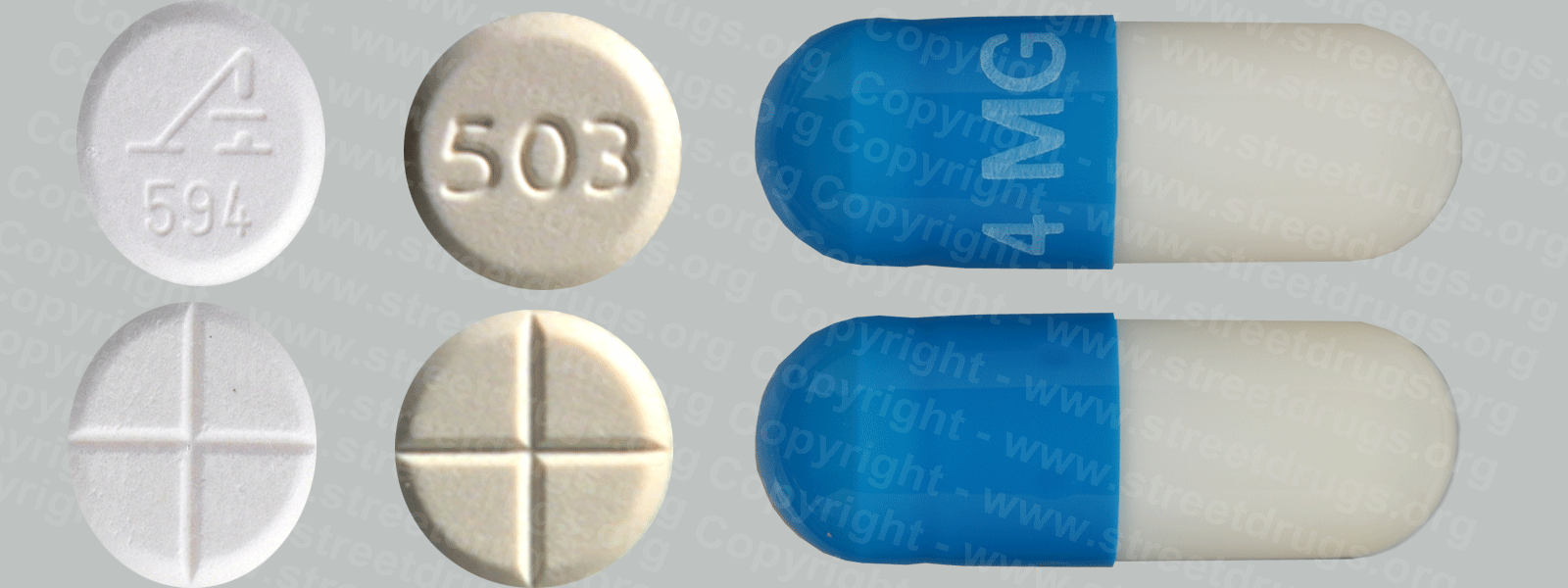
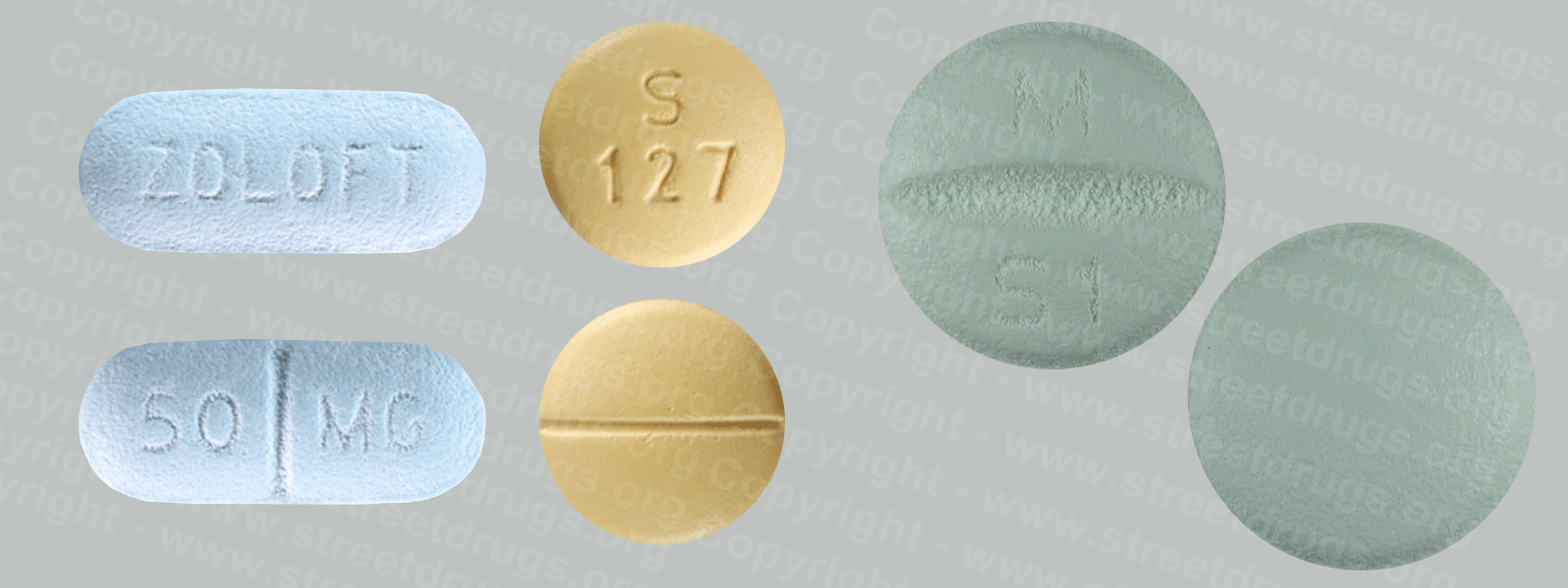
Methamphetamine can be prescribed by a doctor to treat attention deficit hyperactivity disorder and other conditions, although it is rarely used medically, and only at doses much lower than those typically abused. It is classified as a Schedule II drug, meaning it has a high potential for abuse and is available only through a prescription that cannot be refilled.
People who use methamphetamine long-term may experience anxiety, confusion, insomnia, and mood disturbances and display violent behavior. They may also show symptoms of psychosis, such as paranoia, visual and auditory hallucinations, and delusions (for example, the sensation of insects crawling under the skin).
Chronic methamphetamine use is accompanied by chemical and molecular changes in the brain. Imaging studies have shown changes in the activity of the dopamine system that are associated with reduced motor skills and impaired verbal learning. In studies of chronic methamphetamine users, severe structural and functional changes have been found in areas of the brain associated with emotion and memory, which may account for many of the emotional and cognitive problems observed in these individuals.
Some of these brain changes persist long after methamphetamine use is stopped, although some may reverse after being off the drug for a sustained period (e.g., more than 1 year).
Most of the methamphetamine abused in the United States is manufactured in “superlabs” here or, more often, in Mexico. But the drug is also easily made in small clandestine laboratories, with relatively inexpensive over-the-counter ingredients such as pseudoephedrine, a common ingredient in cold medicines. To curb production of methamphetamine, pharmacies and other retail stores are required by law to keep logs of purchases of products containing pseudoephedrine; individuals may only purchase a limited amount of those products on a single day.
Methamphetamine production also involves a number of other, very hazardous chemicals. Toxicity from these chemicals can remain in the environment around a methamphetamine production lab long after the lab has been shut down, causing a wide range of health problems for people living in the area. (See the Methamphetamine Labs link).
What Are the Other Health Effects of Methamphetamine?
Taking even small amounts of methamphetamine can result in many of the same physical effects as those of other stimulants, such as cocaine or amphetamines. These include increased wakefulness, increased physical activity, decreased appetite, increased respiration, rapid heart rate, irregular heartbeat, increased blood pressure, and increased body temperature.
Long-term methamphetamine use has many negative consequences for physical health, including extreme weight loss, severe dental problems (“meth mouth”), and skin sores caused by scratching.
Methamphetamine use also raises the risk of contracting infectious diseases like HIV and hepatitis B and C. These can be contracted both by sharing contaminated drug injection equipment and through unsafe sex. Regardless of how it is taken, methamphetamine alters judgment and inhibition and can lead people to engage in these and other types of risky behavior.
Methamphetamine use may also worsen the progression of HIV/AIDS and its consequences. Studies indicate that HIV causes more injury to neurons and greater cognitive impairment in individuals who are HIV-positive and use methamphetamine than it does in HIV-positive people who do not use the drug.