ADIPEX
Phentermine is similar to an amphetamine. It stimulates the central nervous system (nerves and brain), which increases your heart rate and blood pressure and decreases your appetite.
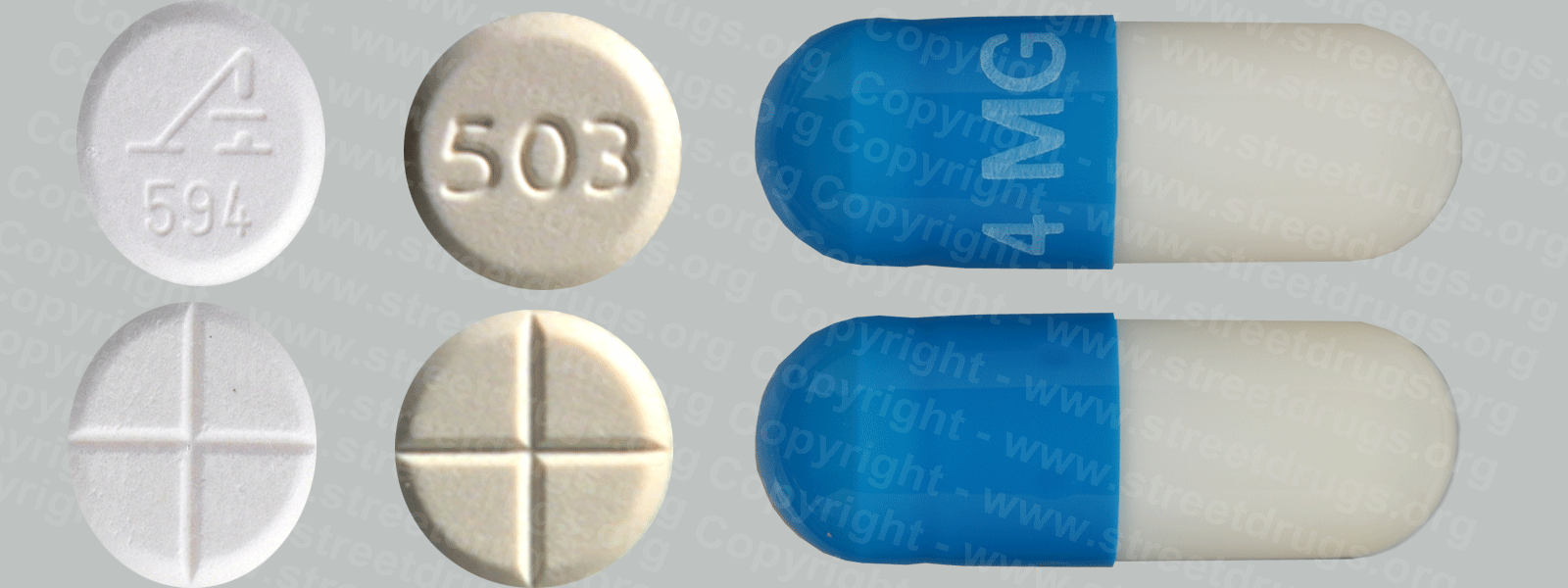
Adipex, (phentermine) is a stimulant that is similar to amphetamine. Phentermine, Adipex, is used for a limited period of time to speed weight loss in overweight people who are exercising and eating a low-calorie diet. Phentermine is in a class of medications called anorectics. It works by decreasing appetite. Phentermine comes as tablets and extended-release capsules. It usually is taken as a single daily dose in the morning or three times a day 30 minutes before meals. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take phentermine exactly as directed. Most people take phentermine for 3 to 6 weeks; the length of treatment depends on how you respond to the medication. Phentermine can be habit-forming. Do not take a larger dose, take it more often, or take it for a longer period than your doctor tells you to. If you are taking the extended-release (long-acting) tablets, do not split, chew, or crush the tablet. There are some tablets that can be crushed and mixed with food.
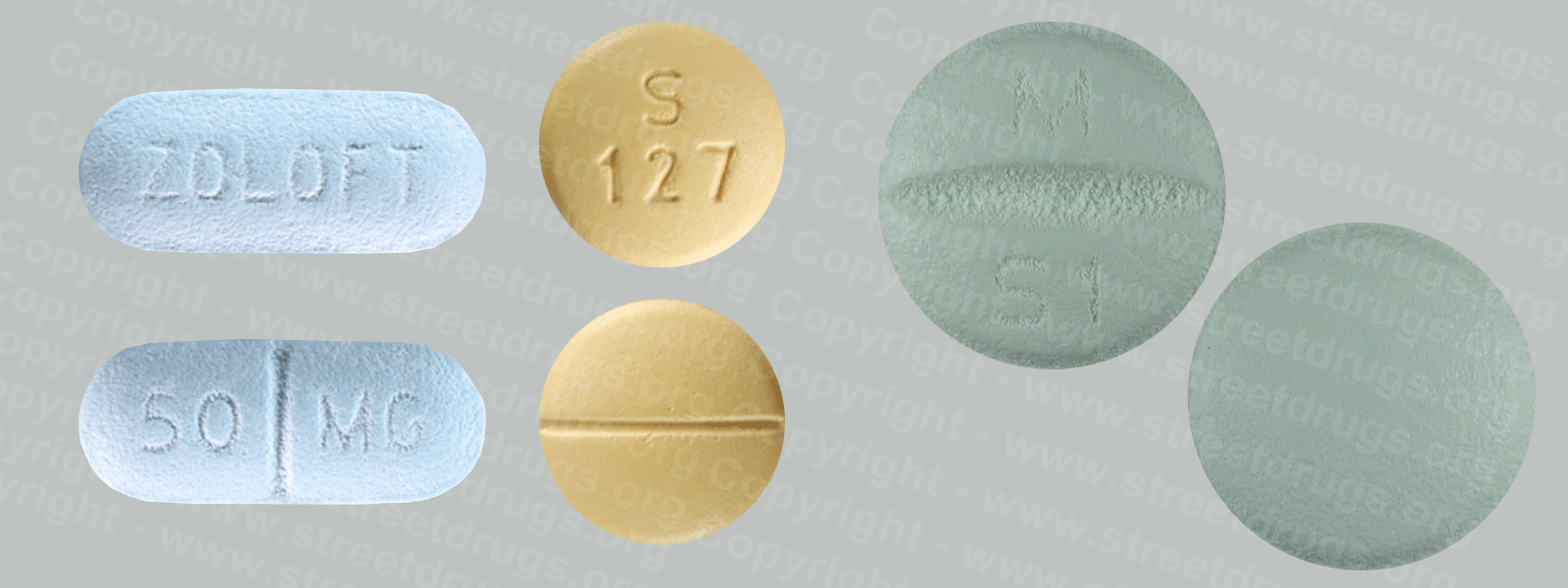
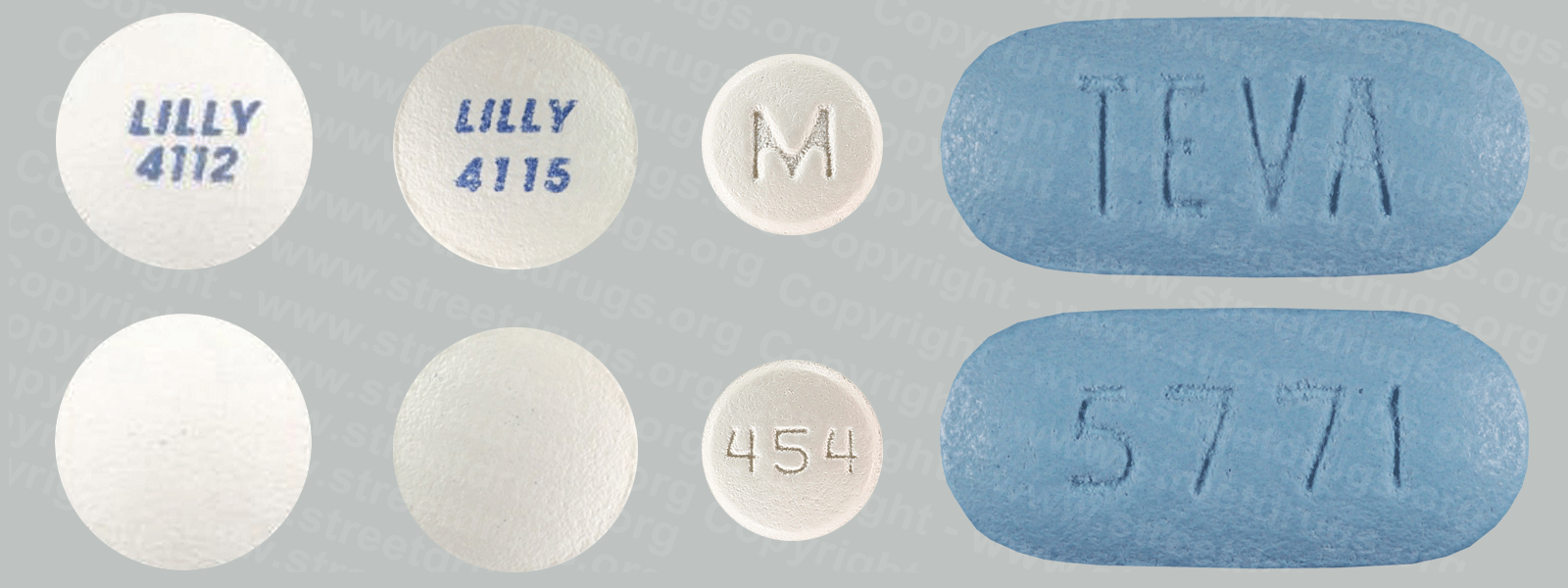
Before taking phentermine tell your doctor and pharmacist if you are allergic to phentermine, any other medications, or any of the ingredients in phentermine tablets. Ask your pharmacist for a list of the ingredients. Tell your doctor and pharmacist what prescription and nonprescription medications, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: fluoxetine (Prozac), fluvoxamine (Luvox), guanethidine, insulin medications for weight loss and depression, paroxetine (Paxil), and sertraline (Zoloft). Also tell your doctor if you are taking monoamine oxidase (MAO) inhibitors such as isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar) and tranylcypromine (Parnate), or if you have stopped taking one of these medications in the past 2 weeks. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
Tell your doctor if you have or have ever had heart disease, high blood pressure, arteriosclerosis (narrowing of the arteries), hyperthyroidism (overactive thyroid gland), diabetes, glaucoma, or a history of drug abuse.
Tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking phentermine, call your doctor. Talk to your doctor about the risks and benefits of taking phentermine if you are 65 years of age or older. Older adults should not usually take phentermine because it is not as safe as other medications that can be used to treat the same condition. You should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you. Ask your doctor about the safe use of alcohol while you are taking phentermine. Alcohol can make the side effects of phentermine worse.If you have diabetes, you may need to decrease your dose of insulin while taking phentermine. Call your doctor if you have questions or problems.
Phentermine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
-dry mouth
-unpleasant taste
-diarrhea
-constipation
-vomiting
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
-increased blood pressure
-heart palpitations
-restlessness
-dizziness
-tremor
-insomnia
-shortness of breath
-chest pain
-swelling of the legs and ankles
-difficulty doing exercise that you have been able to do
See the Prescription Drug Booklet Source: FDA Other Sources Drug Identification GuideCDC FactsCDC Addiction InfoCDC Substance TreatmentSamhsa Workplace Programs Drug-Free Federal Register Codification
CONTACT US
MANUFACTURER LIST