Paxil
axil (Paroxetine) is included in the class of drugs called selective serotonin reuptake inhibitors (SSRIs). This class of drugs is used to treat depression, anxiety, and other mood disorders.
Source: FDA
Use of certain antidepressants, selective serotonin-reuptake inhibitors most commonly known as SSRIs, during pregnancy does not significantly increase the risk for most birth defects, according to a new Centers for Disease Control and Prevention (CDC) study, released today in the New England Journal of Medicine NEJM).
The study, “Use of Selective Serotonin-Reuptake Inhibitors in Pregnancy and the Risk of Birth Defects,” found no significant increase in the risks for the majority of birth defects assessed when all SSRIs were studied together. This finding includes the risk for congenital heart defects, which were associated with SSRI use in previous studies. Researchers, did, however, find associations between SSRI use and three specific birth defects: a defect of the brain, one type of abnormal skull development and a gastrointestinal abnormality. CDC plans to continue to study the association to clarify whether a true risk exists.
“Overall, our results are generally reassuring with respect to the use of antidepressants during pregnancy,” said Jennita Reefhuis, a CDC epidemiologist and one of the authors of the study. “We know that both the mother and baby benefit when a pregnant woman with a serious depressive illness is able to stay on some sort of treatment. The risks may vary for different SSRIs and groups of women. It’s important that women talk with their doctor about the risks and benefits of taking SSRIs during pregnancy.”
Reefhuis noted that while the study found an association between SSRI use and increased risk for three specific birth defects, the increases in risk were minimal and have not been found before. Further, the second study on SSRI and birth defects, also published in the June 28 issue of NEJM, did not find such an association with birth defects overall but did find significant associations between specific SSRIs and several birth defects.
According to Reefhuis, every pregnancy has a 3 percent risk of a major birth defect, regardless of exposures. A woman’s lifetime risk for major depression is 10 percent to 25 percent, with the highest prevalence in childbearing years (18-44 years).
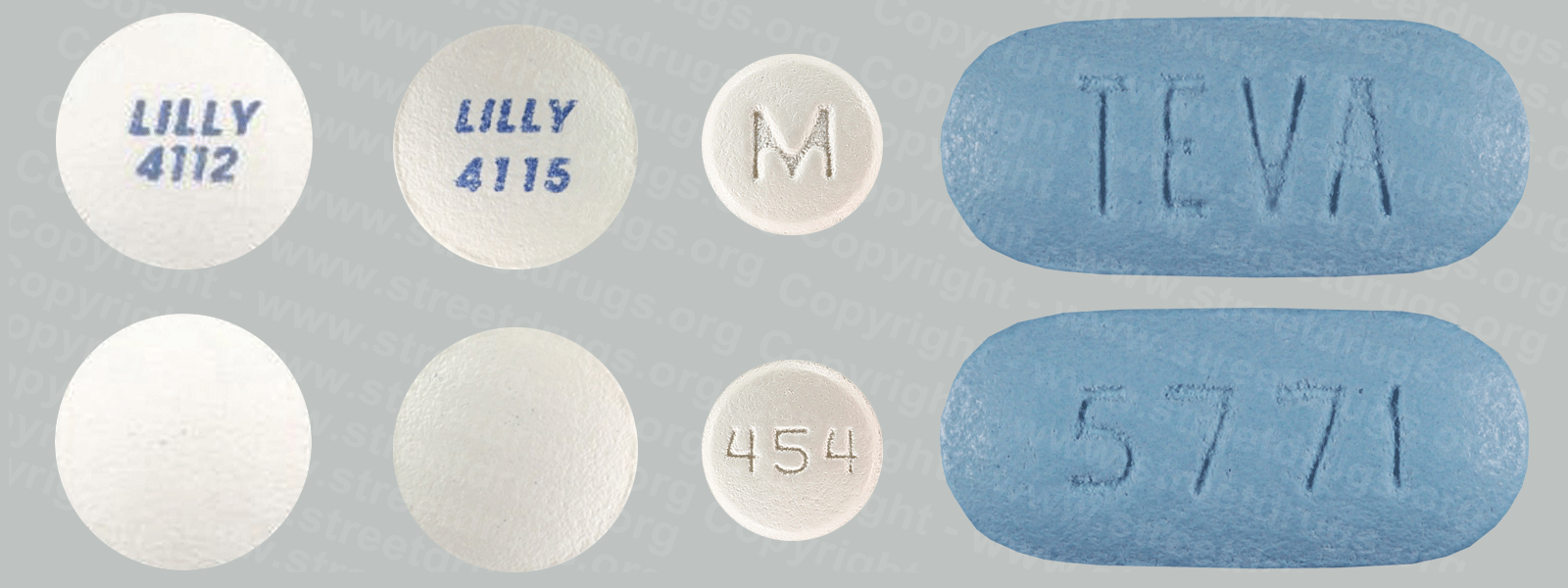
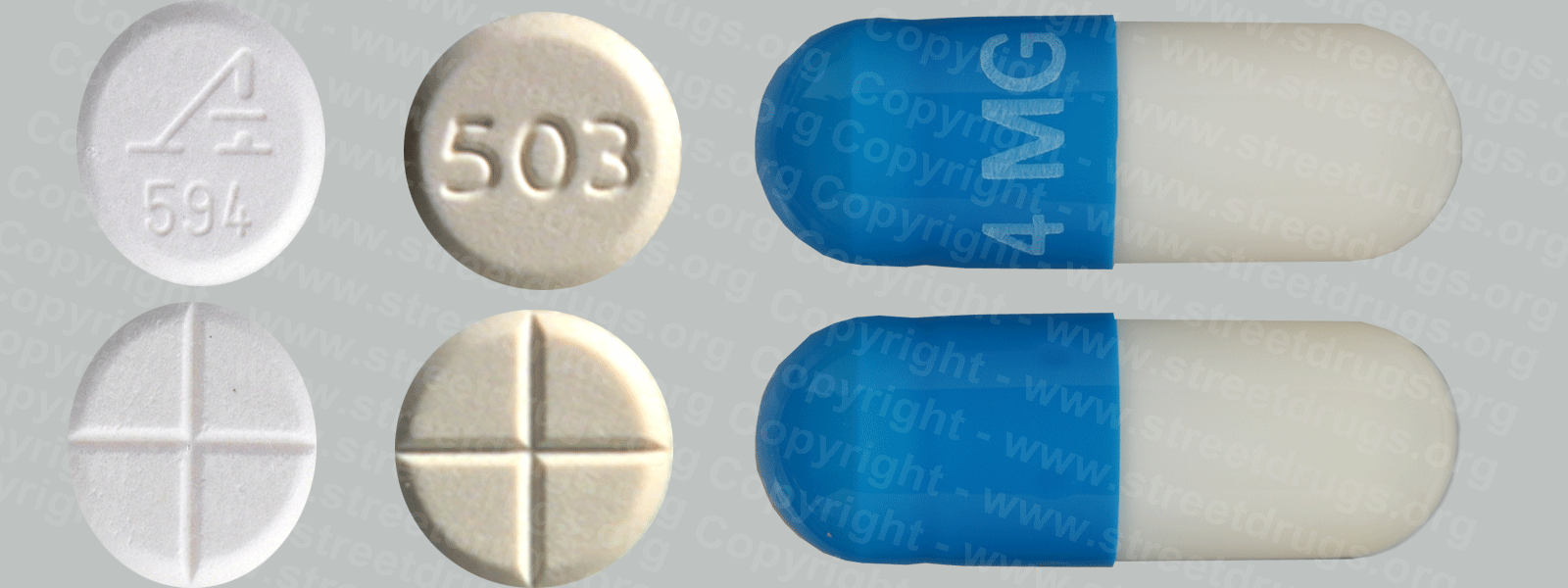
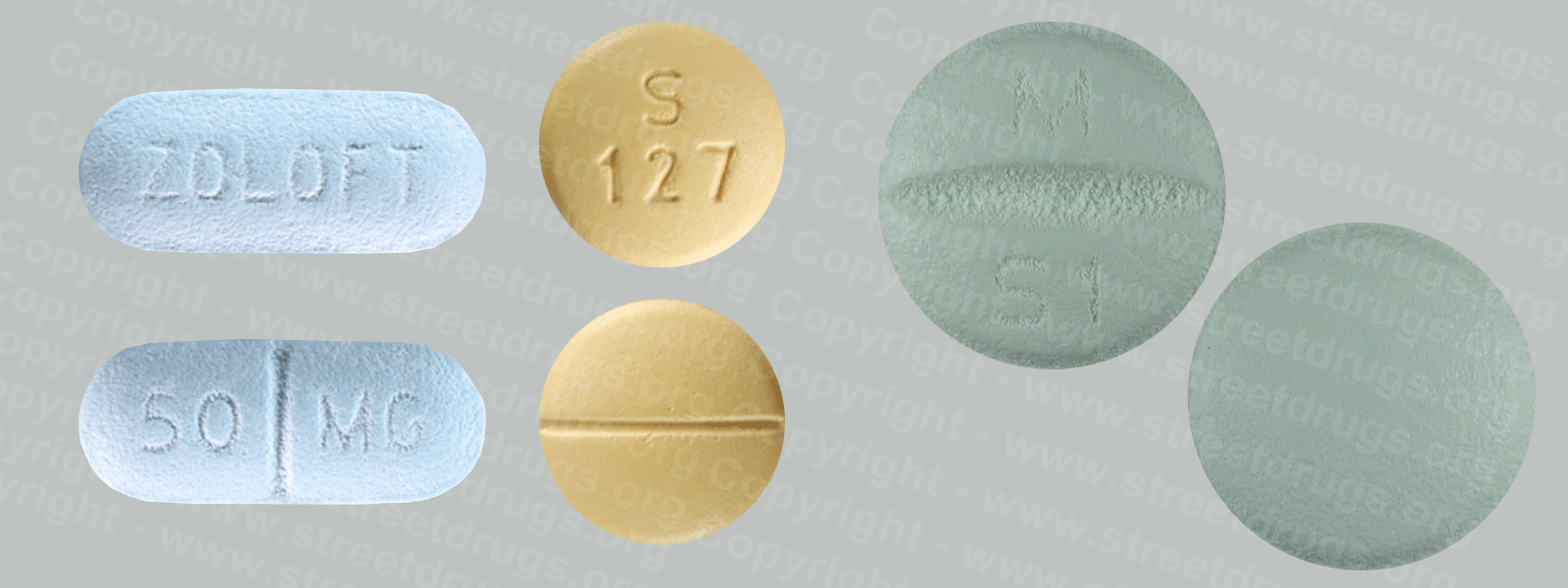
The study examined four SSRIs used to treat such depression—fluoxetine, sertraline, paroxetine, and citalopram—and 18 birth defect categories, including defects of the brain, spine, heart, and mouth. The women in the study took these SSRIs the month before they became pregnant or in the first three months of pregnancy. SSRIs are the most frequently used class of antidepressant medications in general and during pregnancy in the United States, but available data on the safety of SSRI medications in pregnancy has been limited.
The study examined data from 9,622 infants with major birth defects and 4,092 infants without major birth defects, all born during 1997–2002. The data were obtained from the CDC–funded National Birth Defects Prevention Study (NBDPS). The NBDPS is an ongoing study that collects information from the states of Arkansas, California, Georgia, Iowa, Massachusetts, New York, North Carolina, Texas and Utah on the pregnancies of mothers of children with and without birth defects. It is one of the largest epidemiological efforts ever undertaken in the United States to identify causes of birth defects.
Reefhuis noted that as with all medications, CDC’s overall recommendation is that women carefully review the potential benefits and risks of SSRI treatment with their doctor so they can make informed decisions about therapies.
Genomics|Genetic Testing|EGAPP Recommendations|CYP450 …
www.cdc.gov/genomics/gtesting/EGAPP/recommend/CYP450.htm
CYP450 Genotyping to Predict Response to SSRIs Used to Treat Non-psychotic Depression in Adults: EGAPP™ Recommendation
Meningitis | About Bacterial Meningitis Infection | CDC
www.cdc.gov/meningitis/bacterial.html
Bacterial meningitis is usually severe. While most people with meningitis recover, it can cause serious complications, such as brain damage, hearing …
General Public: CYP450 Genotyping and Use of SSRI Drugs …