Bath Salts
Synthetic cathinones, more commonly known as “bath salts,” are human-made stimulants chemically related to cathinone, a substance found in the khat plant. Khat is a shrub grown in East Africa and southern Arabia, where some people chew its leaves for their mild stimulant effects. Human-made versions of cathinone can be much stronger than the natural product and, in some cases, very dangerous.
Synthetic cathinones usually take the form of a white or brown crystal-like powder and are sold in small plastic or foil packages labeled “not for human consumption.” They can be labeled as “bath salts,” “plant food,” “jewelry cleaner,” or “phone screen cleaner.”
Synthetic cathinones are part of a group of drugs that concern public health officials called “new psychoactive substances” (NPS). NPS are unregulated psychoactive mind-altering substances with no legitimate medical use and are made to copy the effects of controlled substances. They are introduced and reintroduced into the market in quick succession to dodge or hinder law enforcement efforts to address their manufacture and sale.
Synthetic cathinones are marketed as cheap substitutes for other stimulants such as methamphetamine and cocaine, and products sold as Molly (MDMA) often contain synthetic cathinones instead.
People can buy synthetic cathinones online and in drug paraphernalia stores under a variety of brand names, which include:
Bliss
Cloud Nine
Lunar Wave
Vanilla Sky
White Lightning
How do people use synthetic cathinones?
People typically swallow, snort, smoke, or inject synthetic cathinones.
How do synthetic cathinones affect the brain?
Much is still unknown about how synthetic cathinones affect the human brain. Researchers do know that synthetic cathinones are chemically similar to drugs like amphetamines, cocaine, and MDMA.
A study found that 3,4-methylenedioxypyrovalerone (MDPV), a common synthetic cathinone, affects the brain in a manner similar to cocaine, but is at least 10 times more powerful. MDPV is the most common synthetic cathinone found in the blood and urine of patients admitted to emergency departments after taking “bath salts.”
Synthetic cathinones can produce effects that include:
paranoia—extreme and unreasonable distrust of others
hallucinations—experiencing sensations and images that seem real but are not
increased friendliness
increased sex drive
panic attacks
excited delirium—extreme agitation and violent behavior
What are other health effects of synthetic cathinones?
Raised heart rate, blood pressure, and chest pain are some other health effects of synthetic cathinones. People who experience delirium often suffer from dehydration, breakdown of skeletal muscle tissue, and kidney failure.
The worst outcomes are associated with snorting or needle injection. Intoxication from synthetic cathinones has resulted in death.
Are synthetic cathinones addictive?
Yes, synthetic cathinones can be addictive. Animal studies show that rats will compulsively self-administer synthetic cathinones. Human users have reported that the drugs trigger intense, uncontrollable urges to use the drug again.
Taking synthetic cathinones can cause strong withdrawal symptoms that include:
depression
anxiety
tremors
problems sleeping
paranoia
How can people get treatment for addiction to synthetic cathinones?
Behavioral therapy can be used to treat addiction to synthetic cathinones. Examples include:
cognitive-behavioral therapy
contingency management, or motivational incentives—providing rewards to patients who remain substance free
motivational enhancement therapy
behavioral treatments geared to teens
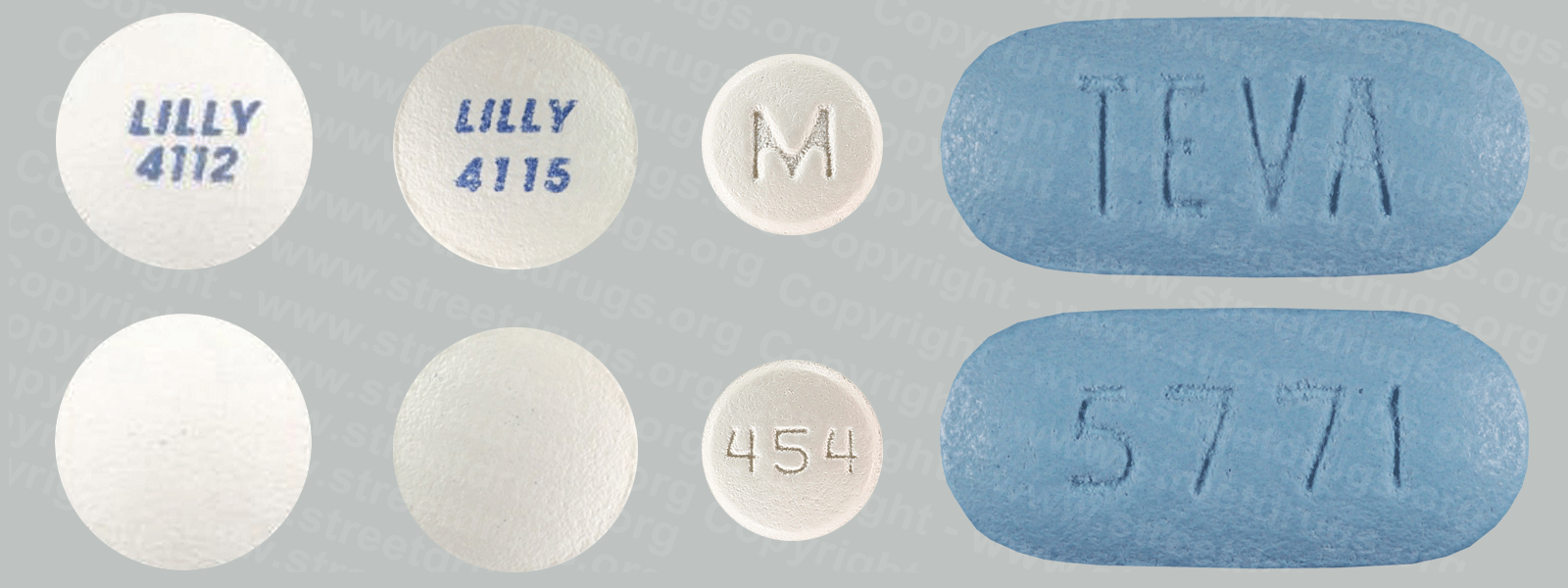
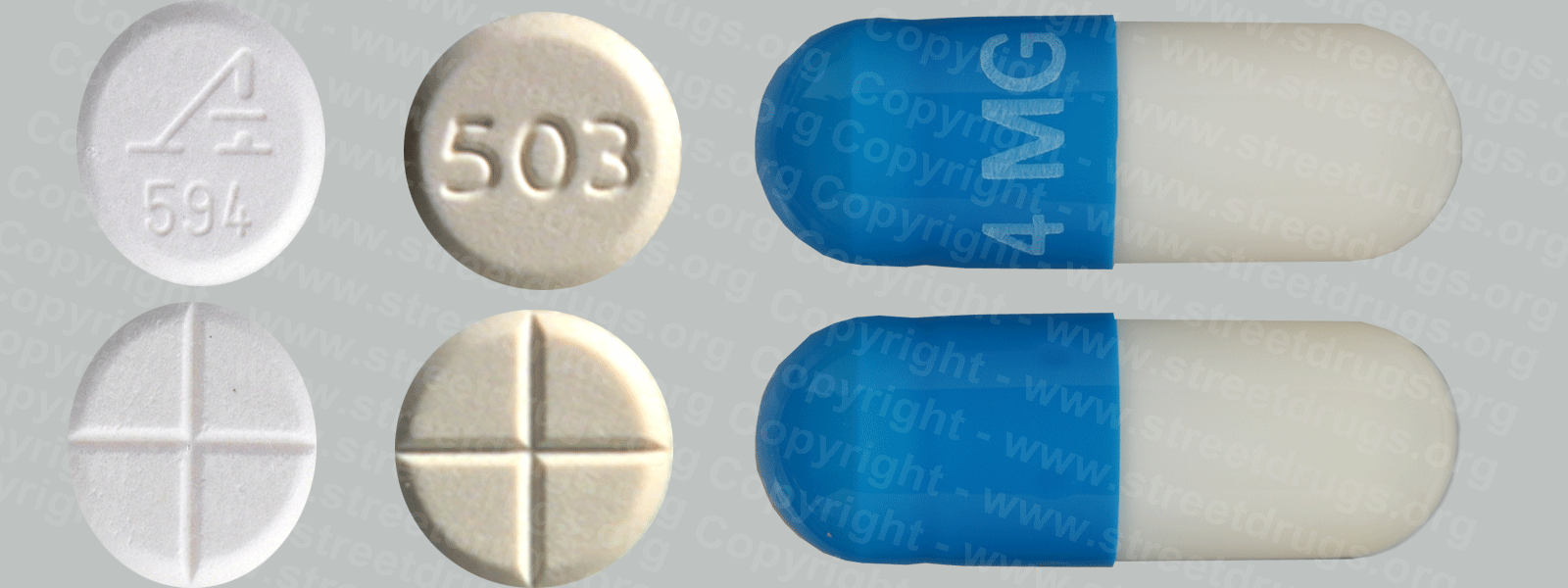
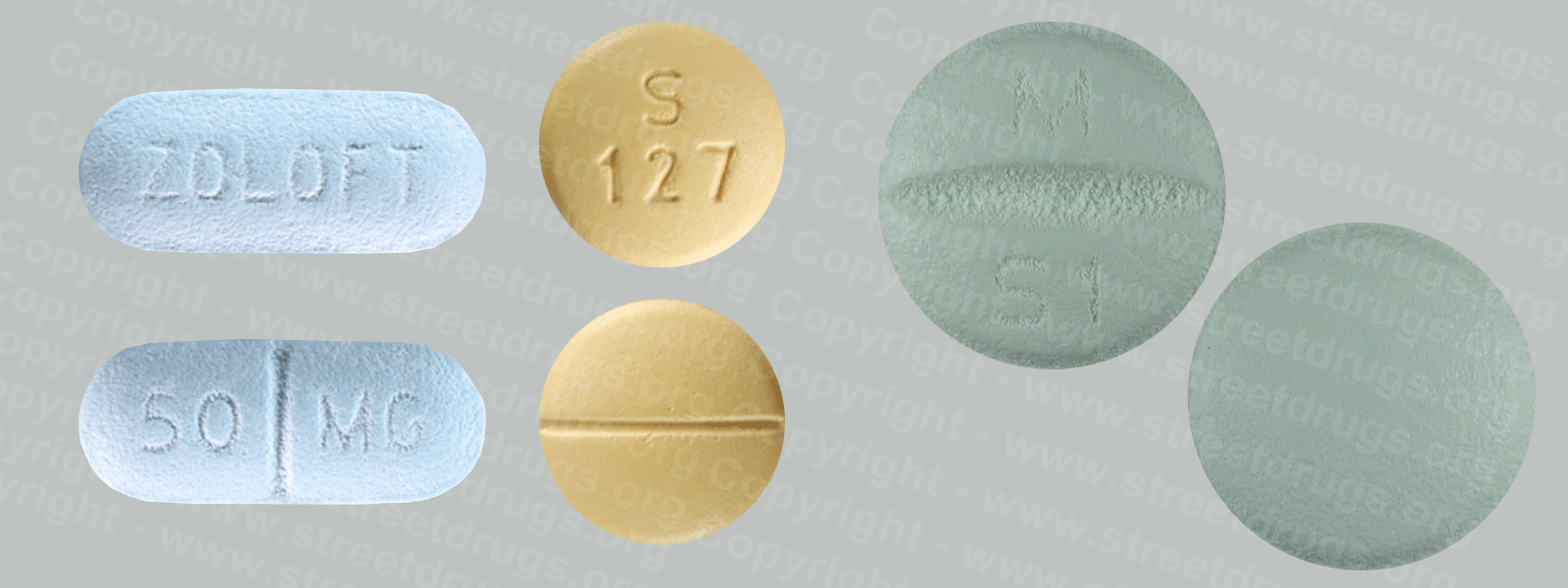
As with all addictions, health care providers should screen for co-occurring mental health conditions. While there are no FDA-approved medicines for synthetic cathinone addiction, there are medicines available for common co-occurring conditions.
Source: NIDA, NIH, U.S. Department of Health and Human Services.